Understanding Your Menstrual Cycle
This blog is to help you learn all about your menstrual cycle, what to expect in each phase, and how to improve the health of your cycle!!
Talking about female reproductive health is still a bit of a taboo subject- sometimes it makes people uncomfortable. We have found that the more we can inform on a subject, the less taboo it feels as we start to understand it! And what better thing for us to understand than our own bodies?! So, let’s dive into learning more about our menstrual cycle!
Menstrual cycle 101
Menstruation typically begins for females between the age of 11-14 or about 2 years after breast development begins (3). Menstruation is paused during pregnancy, and typically ends around 50 years of age on average when menopause begins. A normal menstrual cycle is typically 24-35 days (3), however, it is important to identify what YOUR normal is. We strongly recommend tracking your cycle to learn more about it- the app “flo” is a great place to start if you want to gather general information!
We do want to emphasize- if you are on hormonal birth control, the bleed that you experience each month is NOT a regular period- this is a pill bleed- a bleed that occurs as a result of a withdrawal of hormones (when you stop taking the pill and switch to sugar pills/no pills). If you are on hormonal birth control, you are not ovulating, you are not having a period, and you are not experiencing the rise and fall of hormones that are associated with the menstrual cycle of someone not on birth control. Of course, if you choose to be on birth control, we completely support this decision! However, it is important to be informed!
If you want to read more about this, please checkout this amazing blog by Dr. Lara Briden on this subject: https://www.larabriden.com/why-pill-bleeds-are-not-periods/
When looking at the menstrual cycle, it is important to understand the different phases of the menstrual cycle: The follicular phase and the luteal phase.
Follicular Phase
When you think of the follicular phase, think of F= “First”! This is the FIRST phase of your menstrual cycle, and it begins on day 1 of your cycle, which is the first day of menstruation (your period), and lasts approximately 14 days. The follicular phase is when estrogen is highest, and progesterone is its lowest.
During the follicular phase, women are typically more insulin sensitive, meaning they are better able to use carbs as fuel during this phase. This could potentially explain why some women notice increases in performance in strength training during this phase as carbs are our bodies main source of fuel! If you notice this increase in performance during your cycle, enjoy this time in your training, it is empowering to understand why energy, performance, and other biofeedback changes happen during your cycle!
HOWEVER, studies are currently limited in the area of “training for your menstrual cycle”, and we recommend continuing with your normal programming during both the follicular phase and luteal phase. Instead of proactively changing how you train based on your cycle, instead, understanding WHY your body may be feeling a certain way based on the timing of your cycle, and adjusting intensity IF needed based on how your body is feeling is our recommendation. Strength training based on rate of perceived exertion (RPE) is a helpful guide for appropriate intensity levels during your training. This means aiming to lift weights that are around 8-9/10 on the difficulty scale for you, or to the degree in which you could only lift that weight 1-2 more times with good form before failing.
Estrogen continues to rise throughout this phase, triggering a cascade of hormones that eventually results in you experiencing a spike in follicle stimulating hormone (FSH) and luteinizing hormone (LH), which triggers the follicle (small fluid filled sac) to grow and eventually burst releasing the egg (this is ovulation) within 24-36 hours. Changes in cervical mucus (vaginal discharge) occur during this time. As you get closer to ovulation, cervical mucus changes from dry/sticky, to creamy, to eventually watery/egg white. When it is watery and egg white is when you are likely most fertile, as this cervical mucus is often present right before ovulation. After ovulation, you move into the second phase of your menstrual cycle- the luteal phase.
Luteal Phase:
After ovulation, progesterone is released by the corpus luteum (the leftover follicle) and it increases until it peaks about 5-7 days after ovulation. Progesterone is incredibly important for bone health, brain health, breast health (low serum levels of progesterone have been associated with higher rates of breast cancer)(1), and fertility (you only make progesterone once you ovulate… you need to ovulate to get pregnant). Progesterone also helps thicken the uterine lining and prevents shedding of the uterine lining, allowing time for an embryo to implant and lead to a pregnancy (1).
In the luteal phase, fat oxidation increases. This means, our bodies may be better able to use fat as fuel during this phase, while you become less insulin sensitive, meaning our bodies are less able to use carbs. Resting energy expenditure also increases (our bodies actually burn about 100-200 calories more/day), and protein oxidation increases (this is why it’s important to always eat high protein!). Our body temperature increases as well after ovulation by about 0.3 degrees on average. If you have ever heard of measuring basal body temperature (BBT) when trying to conceive or learn more about cycle, this is why! A sustained rise in BBT can confirm ovulation and that progesterone is rising.
Other symptoms associated with the luteal phase, especially the late luteal phase (about 1 week before period) include: bloating, fatigue, and constipation OR diarrhea (each person reacts differently!). Some women report elevated cravings during this phase as well. To help manage cravings, we recommend choosing options that align with your goals while still honoring 80-20! Have 80% whole foods as a minimum, while still enjoying the occasional treat!
In terms of training during this phase, it seems people who do endurance style training seem to perform better during this phase compared to more glycolytic, fast paced exercise (like HIIT or CrossFit as an example). However, again, we strongly recommend you assess how YOU feel … Instead of proactively reducing training intensity, we recommend decreasing training intensity IF needed by listening to how your body is feeling during this stage of your cycle, and understanding why your body may be feeling a certain way based on the timing of your cycle.
The luteal phase typically lasts 10-14 days, and then progesterone drops (unless pregnant) and you begin your next cycle starting on the first day of menstruation. Tracking the length of your luteal phase is VERY important, especially if your goal is to conceive- if it is less than 10 (ideally 11) days, this may not be enough time for a fertilized egg to implant in your embryo because the lining has already started to shed. Implantation typically happens around day 8-10 after ovulation, so if progesterone has already dropped by this time and the uterine lining is shedding, an embryo cannot implant and a successful pregnancy cannot happen.
*** important note- while the app Flo and other period trackers will give you an “ovulation date”- ovulation cannot be confirmed without tracking basal body temperature (BBT), blood testing progesterone, urine progesterone testing, or a pregnancy (if you got pregnant, you ovulated for sure!).
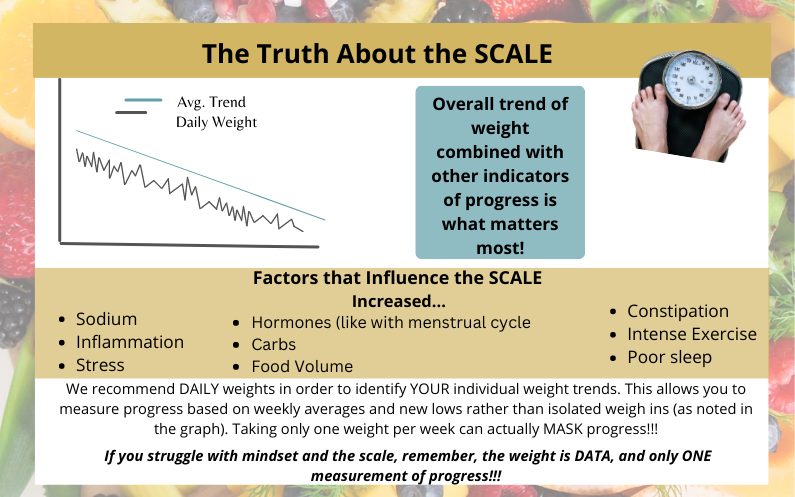
Scale changes throughout the menstrual cycle
It is incredibly common to see scale changes throughout the menstrual cycle, and so wanted to dive into when and why this may be happening.
The first increase in the scale may be during menstruation (typically day 1-5 of cycle). During a women’s menstrual cycle, hormone fluctuations can cause some women to experience constipation and retain more water, which may show up on the scale.
During ovulation- this is an incredibly energy demanding process, with large surges in hormones occurring, specifically in estrogen, follicle stimulating hormone, and lutenizing hormones. These hormones can again cause some women to experience bloating, constipation, and water retention.
During the late luteal phase (about one week before your menstruation begins), progesterone is at its highest which may cause bloating, constipation, and water retention.
So, as you can see… there are a LOT of fluctuations that women experience during the menstrual cycle when it comes to hormones which may influence weight. This is why we strongly recommend comparing weight by weekly averages and monthly averages and looking at the trend. So for example, say your cycle is about 30 days usually, compare the same day this month to same day last month, ie: compare weight on september 30th to weight on October 30th. This will allow you to see more accurately if you are maintaining your weight (within 1-3 lbs fluctuation), losing weight (a great goal would be a 2 lbs difference which is 0.5lbs/week) or gaining weight (typically after a rate of 1-2 lbs/month or 0.25-0.5 lbs/week).
5th Vital Sign
Your period/menstrual cycle is a health marker – often referred to as your “5th vital sign”
When you miss a menstrual cycle, there is often a reason for this, and is something worth exploring – here are some common causes of missed cycles
-Pregnancy – whether or not you are trying to conceive, this is definitely one of the first things to check with a pregnancy test to confirm if you are pregnant.
-Amenorrhea Post BCP-this is the absence of your menstrual cycle after long term birth control use. It can take some time to resume your menstrual cycle or experience regularity with your menstrual cycle – the length of time varies for each woman, but is something to be aware of when you stop taking hormonal birth control. Tracking your cycle can be very beneficial during this transition.
-Secondary Amenorrhea or Hypothalamic Amenorrhea – absence of regular menstrual cycle for 3 months or more due to stress (5). Stress can be caused by multiple factors, most common being low calorie dieting, low body weight, and high lifestyle stressors (what defines “low” calorie and low body weight varies for each woman).
When your body perceives there is a great deal of stress it pushes into higher cortisol production while also down regulating the mechanisms that lead to reproduction – decreasing production of your sex hormones (4). If you think of this from an evolutionary standpoint, when life stressors are high, reproduction is put on hold until the stressor is taken care of.
In women with HA, the Endocrine Society recommends correcting the energy imbalance to improve hypothalamic–pituitary–ovarian (HPO) axis function; this often requires behavioral change, including improving energy balance (increasing calories to maintenance), and/or improved nutrition (enhanced micronutrient delivery), decreased exercise activity, and weight gain as necessary (5)
-RED-S – (Relative Energy Deficiency in Sport) (previously called the Female Athlete Triad) – common in female athletes due to low energy availability (LEA). LEA is due to a combination of undereating, overtraining, and under recovery that is associated with low bone density, menstrual health irregularities, increased risk of injury, and many other negative physiological consequences (6). Treatment for this is similar to that of HA.
-Polycystic Ovarian Syndrome (PCOS) – PCOS is a hormonal womens health condition associated with chronic anovulatory cycles, infertility and hormonal imbalances. This often manifests clinically by irregular cycles, hair growth, and acne, amongst other symptoms. There are multiple causes of PCOS (often overlapping) including insulin resistance, inflammation, high androgens, oxidative stress, and gut dysbiosis. If you have been diagnosed with PCOS, identifying the root cause and adjusting lifestyle factors is a key part of your journey.
Note – doctors often recommend the birth control pill in response to menstrual cycle irregularities, however, as mentioned before, a bleed induced by the birth control pill is NOT a true menstrual cycle, it is a withdrawal bleed, so often does not actually treat the root cause of the missing cycle. We encourage you to advocate for your health, and seek out a practitioner who is willing to help you treat the root cause of the issue you are experiencing.
Our top tips to improving menstrual cycle health:
SPEND THE MAJORITY OF THE YEAR EATING AT MAINTENANCE CALORIES.
This is important! Our bodies need FOOD to feel safe enough to ovulate and have a regular menstrual cycle. If you have been missing your menstrual cycle, assessing your energy availability is extremely important – this is a combination of food intake (enough calories) and appropriate training frequency/volume. Below is an image highlighting the different phases of energy balance – note how the maintenance phase is the majority of the year with short and focused fat loss phases IF needed/desired.
2. EAT PROTEIN AT EACH MEAL
Having protein at each meal can help with blood sugar balance which helps lower inflammation. Females eggs are very sensitive to inflammation, and high inflammation has been associated with lowered egg quality. After ovulation, the ruptured follicle becomes the corpus luteum which produces progesterone and estrogen, and if the follicle is damaged or of lower quality, it may not produce enough progesterone after ovulation.
3. EAT MINIMUM 3 CUPS VEGETABLES PER DAY
Veggies are packed with micronutrients that help support our bodily systems, including our menstrual cycle. Getting a variety of vegetables is important, such as leafy greens (spinach, kale, etc) and cruciferous vegetables (broccoli, cauliflower, etc), as well as others! An easy way to hit this goal is to have 1 big salad/day, or have 1 cup of veggies with each meal!
4. MOVE YOUR BODY EVERY DAY
Our bodies were made to move! Moving our bodies daily helps support blood sugar balance, weight maintenance and energy balance, and may also lower premenstrual symptoms like cramping and bloating. We recommend strength training 3-5 times per week with daily low intensity movement such as walking, and cardiovascular training based on personal preference for heart health benefits.
5. EAT ENOUGH HEALTHY FATS (we recommend for females at least 60g/day to support hormone health when at maintenance calories)
Our hormones like estrogen and progesterone are actually made from the fat we ingest! Fat is also essential for micronutrient absorption as some vitamins can only be absorbed when eaten with a fat source (vitamin A, D, E and K). Some awesome fat sources to include in your diet are: olive oil, avocados, coconut products, salmon, whole eggs, nuts/seeds, red meat, and full fat dairy products.
6. LEARN about YOUR Menstrual Cycle. You are unique, it is important to learn about your cycle!
7. SUPPLEMENTS that may help:
Magnesium bis-glycinate at night and B-100 complex in the morning have both been associated with a decrease in menstrual cycle symptoms (such as cramping) (2).
Another thing that can greatly improve your menstrual cycle health and overall well-being is hiring us as a coach! We will help you implement the above strategies and we work with all of our female clients to help them better understand their cycle if this is something that interests them. We want to help you feel empowered to make decisions that best improve your health and live your life in a way that aligns with your goals! We have multiple clients who have hired us with the goal of trying to conceive, and have supported many clients in achieving a healthy pregnancy! If this is something that you want to learn more about, please book a consult call to discuss your unique goals in detail!
If you would like to learn more, we have also attached some additional resources below!
Period Repair Manual by Lara Briden
Beyond the Pill by Jolene Brighton
Taking Charge of your Fertility by Toni Weschler